Toxicities of Novel Anticancer Agents
Authors: Atul Shinagare, Richard Thomas ,Katherine Krajewski
Date: January 11, 2021
Three major classes of novel anticancer agents
- Molecular targeted therapy (MTT)
- Antiangiogenic: VEGF inhibitors
- Non-antiangiogenic: EGFR, BRAF, mTOR inhibitors
- Immune checkpoint inhibitors
- Anti–CTLA-4: ipilimumab
- Anti–PD-1 and PD-L1: Nivolumab, Pembrolizumab
- Hormonal agents
Toxicities of novel anticancer agents
- Dependent on mechanism of action
- Often subtle appearance
- Prompt detection and communication still important
- Some toxicities may serve as biomarker of response
Common toxicities of molecular targeted therapy
| Organ | Findings |
|---|---|
| Bowel | Enterocolitis, pneumatosis, perforation, anastomotic dehiscence, tumor-bowel fistula |
| Liver | Hepatic steatosis |
| Lungs | Pneumonitis, pulmonary hemorrhage |
| Pancreas | Pancreatitis |
| Gallbladder | Sludge, gallbladder wall edema, cholecystitis |
| Kidney | Crizotinib-associated cysts, infarcts |
| Vessels | Thromboembolism (PV thrombus, DVT, PE), hemorrhage |
| Sof Tissues | Fluid retention – ascites, pleural effusion, anasarca |
Bowel Complications
Mechanism
|
 |
|
Colitis
|
  |
|
Pneumatosis and Perforation
Anastomotic Dehiscence
|
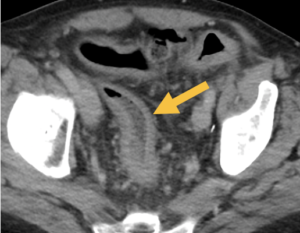
Patient with pneumatosis on antiangiogenic therapy  
Resolution of pneumatosis after treatment stopped
|
|
Tumor-bowel Fistula
|
 
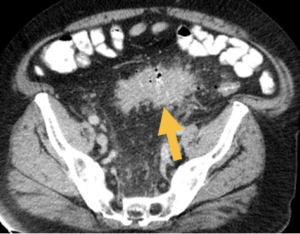
Patient with ovarian cancer: Tumor-bowel fistula on bevacizumab |
Other Toxicities of Molecular Targeted Therapy
|
Pneumonitis
|
 Patient RCC on everolimus with pneumonitis and colitis |
||
|
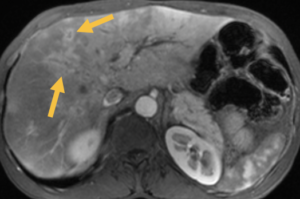
Hepatic Toxicity: Hepatic Steatosis (fatty liver)
Note: Steatohepatitis (Irinotecan) and veno-occlusive disease (Oxaliplatin) common with colon and pancreatic cancer patients Occasionally focal fatty change may mimic metastases
|
|
||
|
Pancreatitis
|
 Pancreatitis on sunitinib |
||
|
Vascular Complications
|
|
||
|
Fluid Retention
|
 Fluid retention in patient with imatinib |
- Immune-related adverse events (irAEs) are immunologic “flare” phenomenon
- Clinically any grade irAEs in 72%; high-grade in 24%
- On imaging: 31% with ipilimumab, 14% with nivolumab
- Colitis (12-19%), pneumonitis (5%), sarcoid-like reaction (5%)
- Treatment steroids
Common toxicities of immune checkpoint inhibitors
| Organ | Findings |
|---|---|
| Bowel | Enterocolitis |
| Liver | Hepatitis, cholangitis |
| Lungs | Pneumonitis |
| Lymph Nodes | Sarcoid-like reaction |
| Pancreas | Pancreatitis |
| Endocrine | Hypophysitis, thyroiditis, adrenalitis |
|
Immune-mediated Colitis
Patterns of Colitis: Diffuse Colitis
Segmental Colitis
|
|
|
Immune-mediated Pneumonitis
|
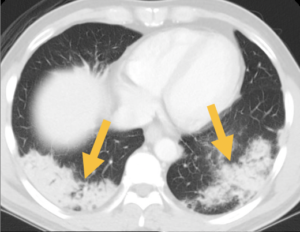 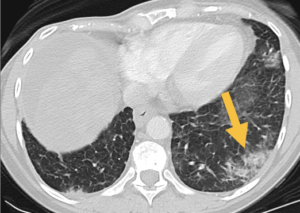 Two different patients with immune-mediated pneumonitis |
|
Sarcoid-like Reaction
|
 Thoracic lumphadenopathy, pulmonary nodules and splenic uptake at 3 months that resolved spontaneously |
|
Immune-mediated Hepatitis
Immune-mediated Cholangitis
|
|
|
Immune-mediated Pancreatitis
|
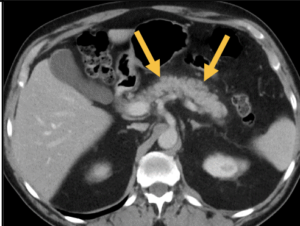 Diffuse peripancreatic stranding from immune-mediated pancreatitis in patient being treated with pembrolizumab |
|
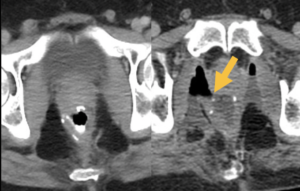
Endocrine irAE
|
 Bulky heterogeneous thyroid in a patient on nivolumab with hoarseness of voice |
|
Vascular Thromboembolism
|
 |
|
Pneumatosis, AVN
|
|
|
Endometrial Changes
|
 Endometrial hyperplasia in a patient with breast cancer treated with tamoxifen |
Drug Class-based Approach
| Antiangiogenic agents | Bowel complications Hepatic steatosis Pancreatitis Vascular complications, fluid retention |
| mTOR inhibitors | Pneumonitis Enteritis |
| Immune checkpoint inhibitors | Colitis Pneumonitis Sarcoid-like reaction Hepatitis, cholangitis Pancreatitis Endocrine events |
| Hormonal therapy | Vascular Thromboembolism Pneumatosis Avascular necrosis Endometrial changes |
Toxicity Checklist-based Approach
| Brain, Head and neck | Hypophysitis Thyroiditis |
| Chest | Lungs: Pneumonitis Mediastinum: Sarcoid-like reaction Vascular: Hemorrhage, pulmonary embolism, fluid retention (pleural effusion, subcutaneous edema) |
| Abdomen and Pelvis | Bowel: Enterocolitis, pneumatosis, perforation, tumor-bowel fistula Liver: Steatosis, hepatitis Pancreatitis, cholecystitis Vascular: Arterial or venous thromboemboli, infarcts, hemorrhage, fluid retention (ascites, subcutaneous edema) |
- Alessandrino et al. Frequency and imaging features of abdominal immune-related adverse events in metastatic lung cancer patients treated with PD-1 inhibitor. Abdom Radiol (NY). 2019 May;44(5):1917-1927.
- Dabydeen et al. Pneumonitis associated with mTOR inhibitors therapy in patients with metastatic renal cell carcinoma: incidence, radiographic findings and correlation with clinical outcome. Eur J Cancer. 2012 Jul;48(10):1519-24.
- Kim et al. Ipilimumab-associated colitis: CT findings. AJR 2013 May;200(5):W468-74.
- Nishino et al. Anti-PD-1 Inhibitor-Related Pneumonitis in Non-Small Cell Lung Cancer. Cancer Immunol Res. 2016 Apr;4(4):289-93.
- Parithivel et al. Everolimus- and temsirolimus-associated enteritis: report of three cases. J Clin Oncol. 2011 May 10;29(14):e404-6.
- Shinagare et al. Pneumatosis intestinalis and bowel perforation associated with molecular targeted therapy: an emerging problem and the role of radiologists in its management. AJR 2012 Dec;199(6):1259-65.
- Tirumani et al. Tumor-bowel fistula: what radiologists should know. Abdom Imaging. 2013 Oct;38(5):1014-23.
- Tirumani et al. Radiographic Profiling of Immune-Related Adverse Events in Advanced Melanoma Patients Treated with Ipilimumab. Cancer Immunol Res. 2015 Oct;3(10):1185-92.




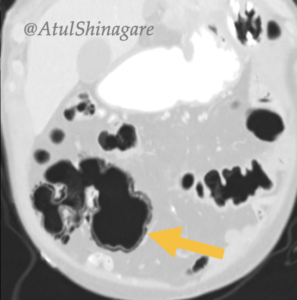
 Pulmonary embolism
Pulmonary embolism