MRI Rectal Cancer Staging
Authors: Shanna A. Matalon, Leslie K Lee, MD, Atul Shinagare, MD, Michael H Rosenthal, MD, Ramin Khorasani
Date: May 24, 2020
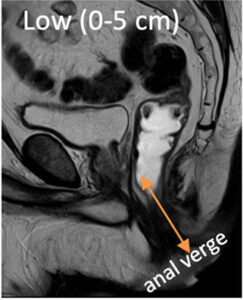
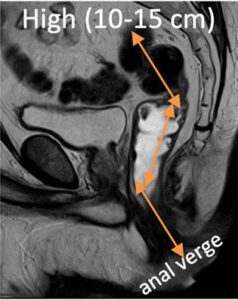
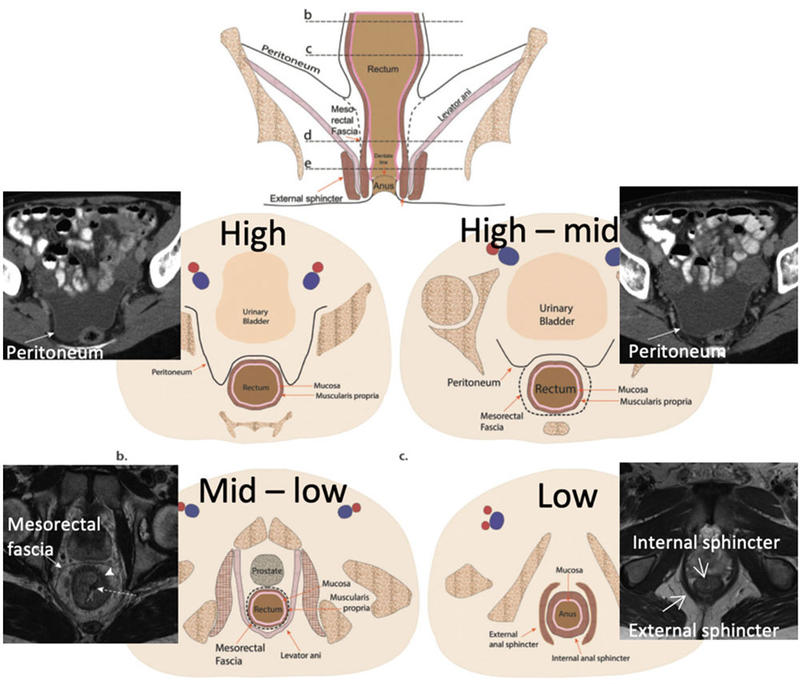
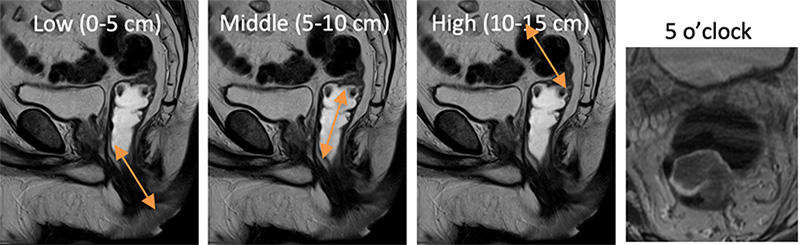
3 Segments (measured from anal verge)

Relationship to Anterior Peritoneal Reflection* and Mesorectal Fascia
- Sigmoid: entirely intraperitoneal
- High rectum: covered by peritoneum anteriorly & laterally
- Mid rectum: covered by peritoneum reflection only anteriorly
- Distal rectum: entirely extraperitoneal, surrounded by mesorectal fascia, which tapers distally and fuses with anal sphincter
* identified in ~70-80% of pelvis MRIs

Images used with permission from Matalon et al. RadioGraphics, 2015.
Identifying the rectosigmoid junction
- Sigmoid is entirely intraperitoneal
- Upper/mid rectum covered anteriorly by peritoneal reflection
- Various definitions exist:
- Top of sacral promontory
- 5 cm above peritoneal reflection
- Confluence of teniae coli (anatomic landmark, not seen by imaging)
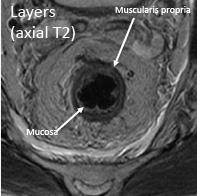
Layers
- Mucosa (innermost layer), submucosa, muscularis propria* (outer dark black line)
- *relevant in T-staging
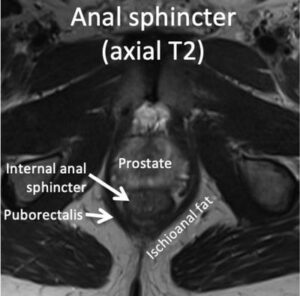
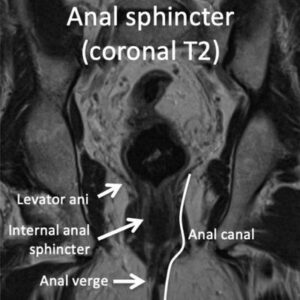
Anal sphincter
- Definitions:
- Internal sphincter: continuation of inner circular layer of muscularis propria
- External sphincter complex: continuation of outer longitudinal layer of muscularis propria, levator ani and puborectalis
- Anal canal: measures between 3-5 cm; anorectal ring to anal verge (surgical definition)
- Anal verge: distal end of anal canal, at junction of anal squamous mucosa and perianal skin
- Anal margin: skin within 5 cm radius from anal verge
| Feature | Description |
|---|---|
|
Location |
 |
|
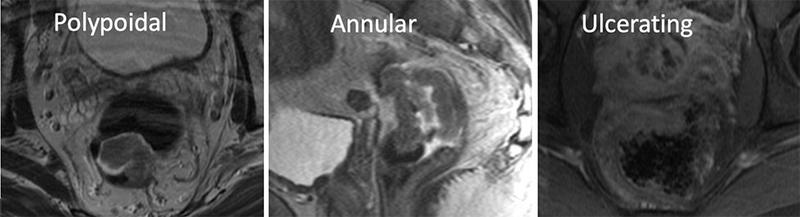
Morphology |
 |
|
Size/length of rectum involved |
|
|
Signal characteristics |
 Describe T1, T2, DWI and enhancement characteristics Describe T1, T2, DWI and enhancement characteristics*High T2 signal suggests mucinous subtype, which tend to have higher metastatic tendency and higher stage at diagnosis |
|
Shortest distance of tumor to mesorectal fascia |
 |
|
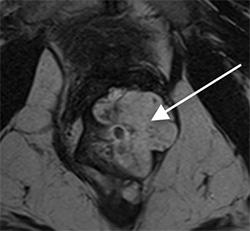
Extramural vascular invasion (EMVI) |
 Look for expanded, T2 intermediate tubular structures in the mesorectal fat or inferior mesenteric vasculature Look for expanded, T2 intermediate tubular structures in the mesorectal fat or inferior mesenteric vasculature
*associated with poorer prognosis, including high risk of local recurrence and higher incidence of nodal and distant metastatic spread |
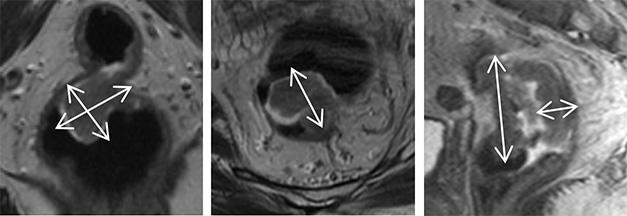
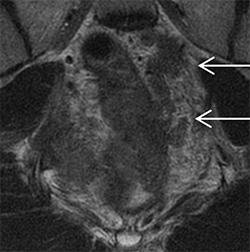
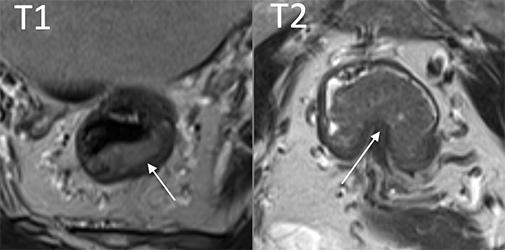
| T Stage |
Examples |
|---|---|
|
T1 (invades submucosa)/T2 (invades muscularis propria, but not beyond) *cannot reliably distinguish by MRI, but may be distinguished by EUS |
 |
|
T3 (invades through muscularis propria into perirectal tissues) |
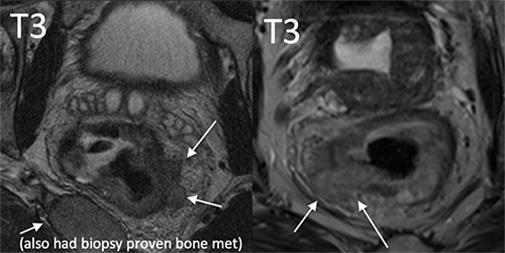 |
|
T4a (invades visceral peritoneum) |
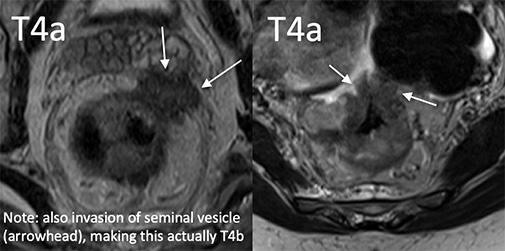 |
|
T4b (tumor invades other organs) |
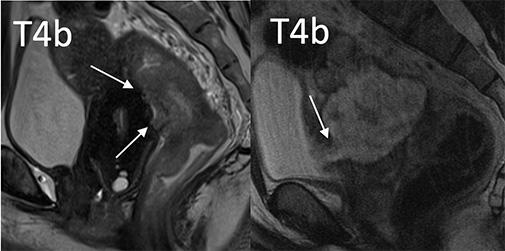 |
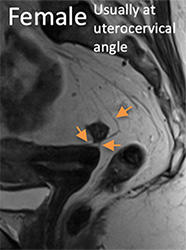
“T” Staging of Low Rectal Tumors*
| T Stage | Examples |
|---|---|
|
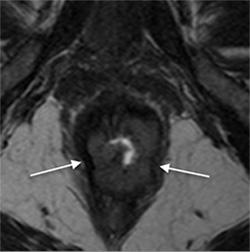
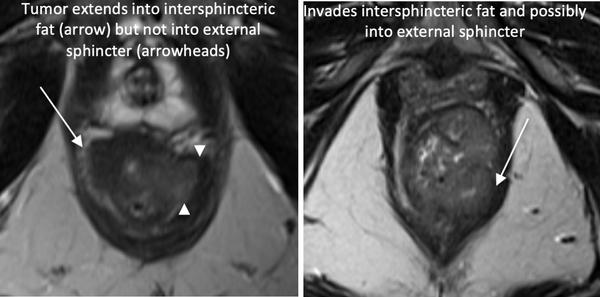
Involves IAS confined to internal anal sphincter |
 |
|
Involves ISS extends beyond internal anal sphincter into intersphincteric space |
 |
|
Involves EAS invades through external sphincter |
 |
|
Invades other organs |
 |
*T-stage not currently recommended by SAR DFP – instead descriptive terms used
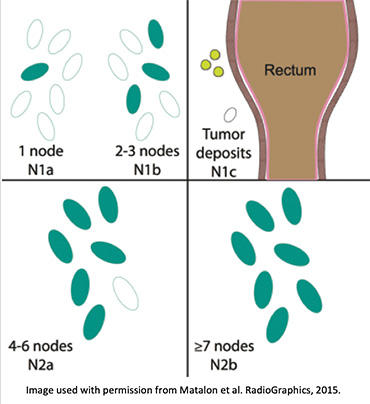
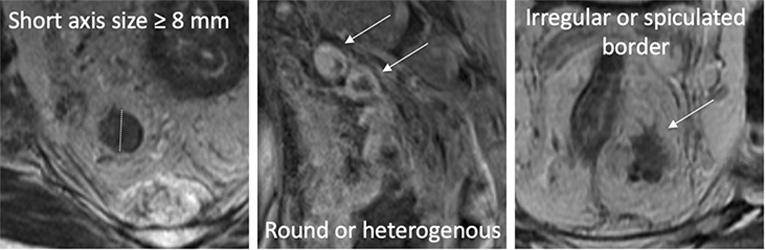
MRI criteria for pathologic lymph nodes:
- Short axis ≥ 9 mm OR
- Size 5-7 mm AND 2 abnormal morphologic features OR
- Size <5 mm AND all 3 abnormal morphologic features
High Yield Sequences
| Sequence | Area of interest |
|---|---|
|
Coronal large FOV T2 |
Screen for metastases |
|
Sagittal T2 |
|
|
Short axis oblique T2 |
T Stage |
|
Long axis oblique T2/coronal T2 |
Relationship to sphincter complex (low cancers) |
|
DWI* *Poor spatial resolution – should not be used for T staging |
|
|
Post contrast** **Not currently recommended per Society of Abdominal Radiology Disease Focused Panel User’s Guide for the Synoptic MRI Report for Pre-Operative Staging of Rectal Cancer 2018 |
May be helpful in distinguishing abnormal morphology lymph nodes |
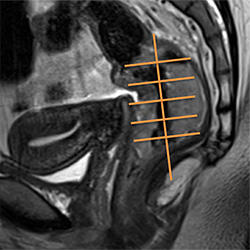
Why and How to Prescribe Oblique Planes
WHY:
- Provides optimal anatomic information
- Reduces T-staging error from volume averaging
HOW:
- Review patient chart to identify location of tumor (clinic notes, endoscopy report, etc, if available)
- Review sagittal T2
- Prescribe planes (fishbone drawing)
- If cannot see tumor:
- Techs can continue scanning through standard planes and review when more images are available
- Prescribe based on described location (low 0-5cm, middle 5-10cm, high 10-15cm)
Sagittal T2

Distinguishing T2 from T3 Disease
1) Beware of volume averaging!
- Always T-stage based off of the oblique planes (reduces potential error from volume averaging) and use other planes as reference to confirm extramural disease
Example 1
| Standard Axial T2 | Oblique Axial T2 |
|---|---|
 |
 |
|
Blurring of muscularis propria with possible extramural tumor (would be T3). |
Clearly intact muscularis propria. Pathology upon resection confirm T2 disease. |
Example 2
| Consecutive Oblique Axial T2 Images | Sagittal T2 | |
|---|---|---|
 |
 |
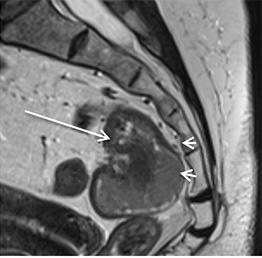 |
|
Loss of dark band of muscularis propria (would be T3 disease). |
Consecutive image(s) showed clearly intact muscularis propria. Attachment site anteriorly (arrow) would make extramural disease posteriorly unlikely. Pathology upon resection confirmed T2 disease. |
Correlative sagittal image shows intact muscularis propria. Attachment site anteriorly (arrow) would make extramural disease posteriorly unlikely. Pathology upon resection confirmed T2 disease. |
Example 3
| Oblique Coronal T2 | Oblique Axial T2 |
|---|---|
 |
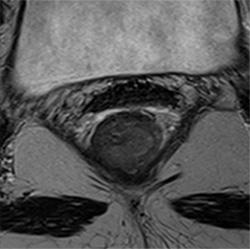 |
|
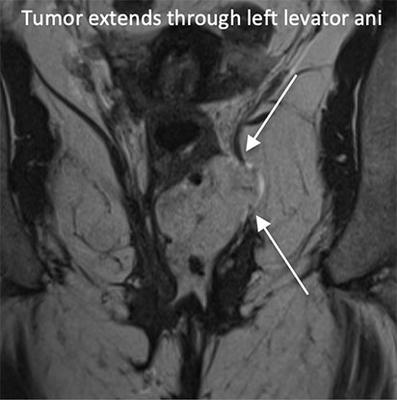
Blurring of the left levator ani (would be T4b disease). |
Correlative axial image shows no tumor outside the internal sphincter, consistent with early T2 disease. |
Example 4
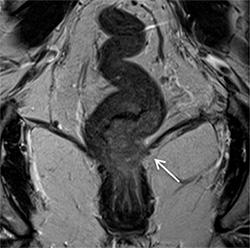
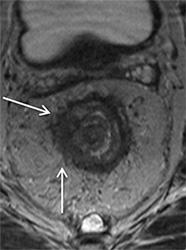
| Oblique Coronal T2 | Oblique Axial T2 |
|---|---|
 |
 |
|
Blurring of the right levator ani (would be T3 disease). |
Correlative axial image shows no tumor extending into the external sphincter, consistent with T2 disease. |
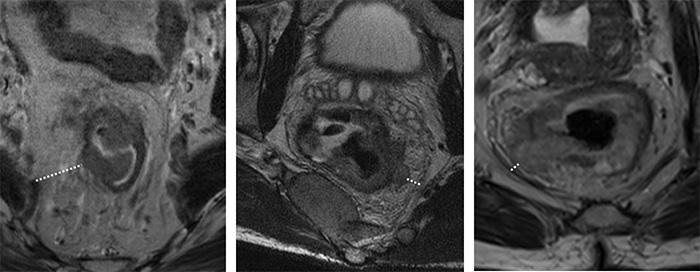
2) Desmoplastic response in T2 tumors versus extramural tumor (T3)
- Desmoplastic response = Linear, spiculated, T2 hypointense signal
- *Often seen in villous adenomas
- Extramural tumor (T3) = masslike, nodular, T2 intermediate signal
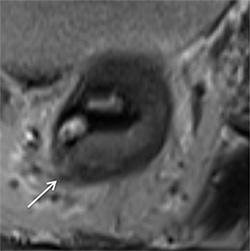
Example 1
| Oblique Axial T2 |
|---|
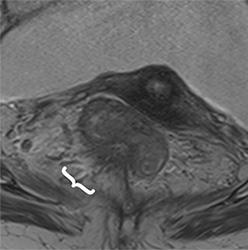 |
|
Pathology proven T2 tumor showing desmoplastic response from 6-9 o’clock (bracket). |
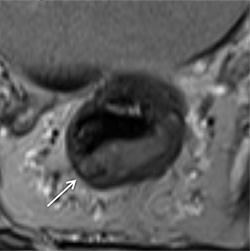
Example 2
| Oblique Axial T2 |
|---|
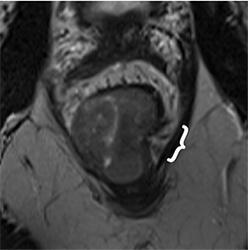 |
|
Pathology proven T2 tumor with desmoplastic response at 3 o’clock (bracket). |
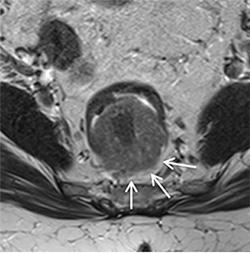
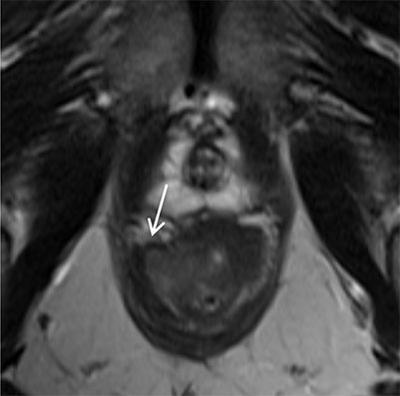
Example 3
| Oblique Axial T2 |
|---|
 |
|
T3 cancer with extension of intermediate T2 signal tumor beyond the muscularis propria from 7-8 o’clock (arrows) AND desmoplastic response (bracket) |
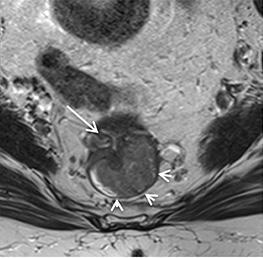
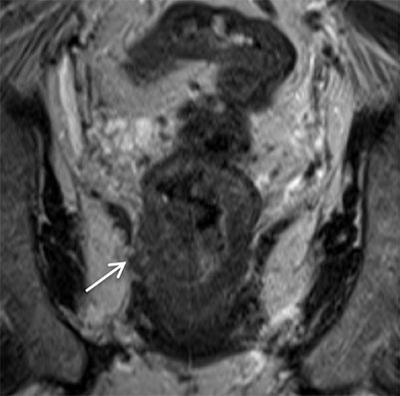
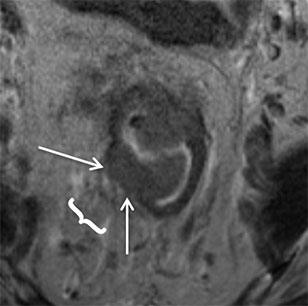
Example 4
| Oblique Axial T2 | Oblique Coronal T2 |
|---|---|
 |
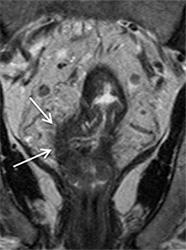 |
|
T3 cancer with extension of intermediate T2 signal tumor beyond the muscularis propria from 7-10 o’clock (arrows) |
|
- Gollub MJ et al. Recognition of the Anterior Peritoneal Reflection at Rectal MRI. AJR. 2013 200:97-101.
- Gollub MJ et al. Current controversy, confusion, and imprecision in the use and interpretation of rectal MRI. Abdominal Radiology. 2019.
- Hope TA et al. Rectal cancer lexicon: consensus statement from the society of abdominal radiology rectal and anal cancer disease-focused panel. Abdominal Radiology. 2019.
- Jhaveri KS & Hooseini-Nik H. MRI of Rectal Cancer: An Overview and Update on Recent Advances. AJR. 2015.
- Kaur H et al. MR Imaging for Preoperative Evaluation of Primary Rectal Cancer: Practical Considerations. RadioGraphics. 2012.
- Matalon SA et al. Anorectal Cancer: Critical Anatomic and Staging Distinctions That Affect Use of Radiation Therapy. RadioGraphics. 2015.
- Nougaret S et al. The use of MR Imaging in Treatment Planning for Patients with Rectal Carcinoma: Have You Checked the “DISTANCE”? Radiology. 2013.