Congenital Uterine Anomalies
Authors: Jessie L. Chai, MD, Kristine S. Burk, MD
Date: May 25, 2020
Embryogeneisis OverviewMullerian Duct Anomalies (MDAs)
- 1-5% of the general population and 13-25% of patients with infertility or recurrent pregnancy loss (1)
- Affecting fallopian tubes, uterus, cervix, and proximal 2/3 of the vagina
- Normal ovaries and distal third of vagina
- Three stages: ductal development, ductal fusion, and septal resorption (2)
Ductal Development
|
Normal:
|
Normal
|
||||
|
Abnormal:
|
Agenesis/Hypoplasia
|
Ductal Fusion
|
Normal: By 10 weeks: paired Mullerian ducts migrating inferiorly and medially, forming uterovaginal canal with midline septum. |
Normal
|
|||
|
Abnormal:
|
|
Septal resorption
|
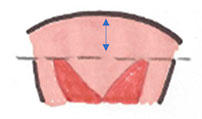
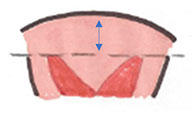
Normal: 9-12 weeks: uterovaginal septum beginning to resorb in bidirectional direction (5). |
Normal
|
|||
|
Abnormal:
|
|
Hysterosalpingography (HSG)
- Limited utility in characterizing Mullerian anomalies since only lumen visualized.
- Pearls: divergent angle of less than 75 degrees between endometrial horns suggesting septate uterus and angle of greater than 105 degrees suggesting bicornuate configuration,
- Pitfalls: overlap between these two entities with majority of cases falling within this range and masses such as adenomyomas or fibroids mimicking these findings (3).
Ultrasound (US)
- 3D imaging useful for visualization of exterior surface of uterine fundus.
- Pearls: imaging during secretory phase preferred when endometrium thicker.
Magnetic resonance (MR)
- Modality of choice since external surface and internal architecture of uterus well depicted.
- T2 weighted sequences for visualization of anatomy–ideally coronal and axial imaging planes prescribed from sagittal images, parallel and perpendicular to body of uterus.
- T1 weighted sequences useful for identification of blood products.
- Large field of view images enabling visualization of kidneys and ureters and any concurrent urinary tract anomalies.
Agenesis or Hypoplasia: Mayer-Rokitansky-Kuster-Hauser Syndrome
- Hypoplasia or agenesis of uterus and upper 2/3 of vagina.
- 5-10% of MDA cases.
- Occurring in 1 out of 4000 females, second most common cause of primary amenorrhea (9).
- Often presenting as primary amenorrhea with normal external characteristics because ovaries functioning normally.
- Rudimentary uterine tissue, if present, always caudal to ovaries which may be ectopic in location (8).
- Once diagnosed, surgery enabling normal sexual function and reproduction occurring with assistance.
Agenesis
|
Vaginal and cervical agenesis |
  |
|
Left renal agenesis in same patient |
 |
Hypoplasia
|
Presumed fibroid (star) stable in size for 14 years and strand of tissue (arrow) which may represent rudimentary uterine tissue |
 |
|
Normal ovaries more superiorly in same patient |
 |
Unicornuate Uterus
|
Unicornuate
|
Unicornuate Uterus without Rudimentary Horn
|
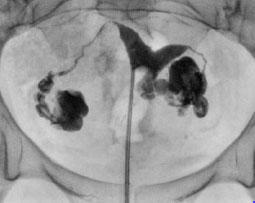
HSG of right unicornuate uterus with patent endometrial cavity and fallopian tube |
 |
|
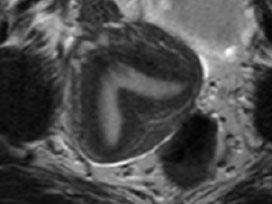
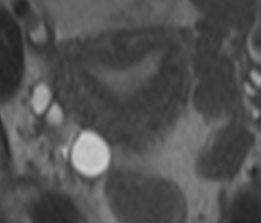
T2 axial MR of left unicornuate uterus |
 |
|
US of right unicornuate uterus |
 |
|
Intrauterine pregnancy in same patient at later date |
 |
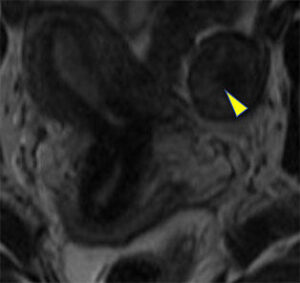
Unicornuate Uterus with Rudimentary Horn
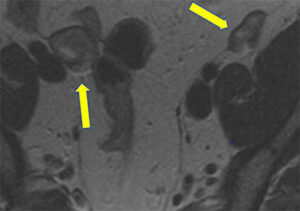
Right unicornuate uterus with rudimentary left horn attached by fibrous tissue (arrow), possible endometrial tissue (arrowhead), and no communication with right endometrial canal
 |
 |
 |
Uterine Didelphys
- Near complete failure of Mullerian duct fusion
- Results in two endometrial cavities, cervixes, and proximal vaginas
- 5% of MDAs (3)
- Pearl: external uterine fundal contour distinguishing fusion failures from incomplete resorption of septum. Bicornuate and didelphys uteri with less than 5 mm myometrium above level of endometrial horns or apex of fundus located below level of horns
|
Septate
|
Bicornuate
|
Bicornuate
|
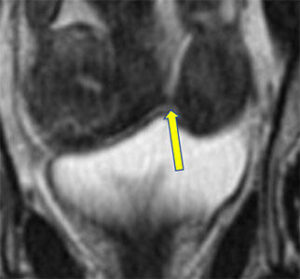
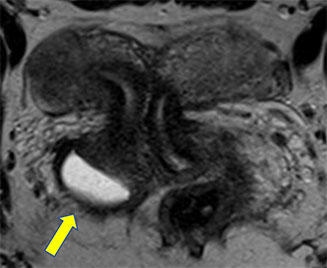
Uterine Didelphys
|
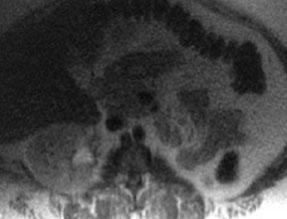
Two endometrial horns (top) Two cervixes (bottom), patient has two proximal vaginas more inferiorly (not pictured) |
  |
|
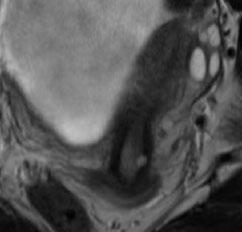
Different patient with fluid collection adjacent to obliterated right hemivagina (arrow), patient subsequently underwent right hysterectomy and salpingectomy |
  |
Bicornuate Uterus
- Incomplete fusion of Mullerian ducts at level of uterine fundus
- Second most common anomaly for MDA infertility patients, accounting for 10% of MDA cases
- Pearl: external uterine fundal contour distinguishing fusion failures from incomplete resorption of septum. Bicornuate and didelphys uteri with less than 5 mm myometrium above level of endometrial horns or apex of fundus located below level of horns
- Pearl: Upper vaginal septa occuring in about 25% of cases and when associated with bicornuate bicollis configuration, difficult to distinguish from didelphys uteri
|
Septate
|
Bicornuate
|
Bicornuate
|
Bicornuate Uterus
|
Apex of fundus below level of uterine horns, two cervixes, and no vaginal septum |
  |
|
Left renal agenesis in same patient |
 |
|
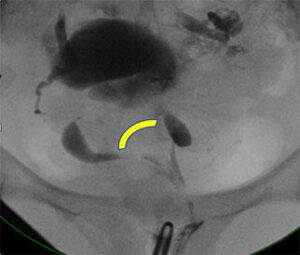
MR and HSG on same patient with wide divergence of endometrial horns on HSG (arc) |
  |
|
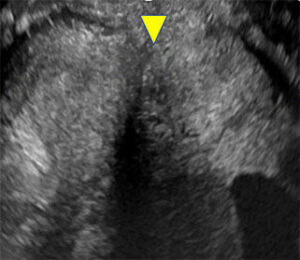
US on different patient with external surface of uterine fundus below level of endometrial horns (arrowheads) |
  |
Septate or Subseptate Uterus
- Normal external contour of uterine fundus
- 55% of MDA cases, poorest reproductive outcome regardless of size of septum (3)
- When complete, extending from uterine fundus through cervix
- Pearl: external uterine fundal contour distinguishing fusion failures from incomplete resorption of septum.
- Septate, subseptate, and arcuate uteri having 5 mm or more of myometrium above level of endometrial horns
- Treatment: Surgical resection of septum
- No residual septum or septum less than 1 cm considered optimal for reproduction
|
Septate
|
Bicornuate
|
Bicornuate
|
Complete Septum
|
Septum extending from fundus through cervix |
 |
|
Same patient with findings more difficult to visualize on coronal CT reformats |
  |
Subseptate Uterus
|
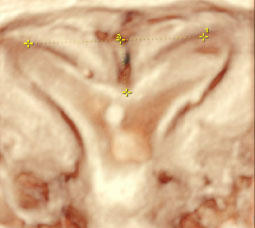
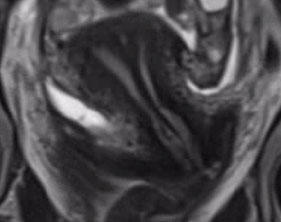
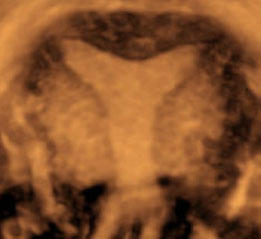
Normal external contour of uterine fundus and divergence of endometrial horns on short axis T2 MR and 3D US |
  |
Post Septate Resection
|
No residual septum or septum less than 1 cm considered optimal for reproduction |
|
||
|
Preoperative MR (left) Postoperative HSG (right) with improved septal abnormality |
  |
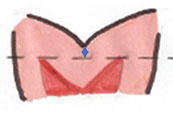
Arcuate Uterus
- Near complete septal resorption
- May be normal variant
- Mild broad indentation of fundal portion of endometrium
- No defining depth to distinguish from broad septum (3)
- Up to 3.9% of general population with no increased prevalence in high risk groups (7)
- Pearl: external uterine fundal contour distinguishing fusion failures from incomplete resorption of septum.
- Septate, subseptate, and arcuate uteri having 5 mm or more of myometrium above level of endometrial horns
|
Septate
|
Bicornuate
|
Bicornuate
|
Arcuate Uterus
|
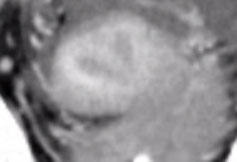
Same patient on MR and 3D US with subtle broad indentation of fundal portion of endometrium with normal external contour of uterine fundus |
  |
- Behr SC, Courtier, JL, Qayyum A. Imaging of Mullerian duct anomalies, Radiographics 2012:32(6)
- Robbins JB, Parry JP, Guite KM et al. MRI of pregnancy-related issues: müllerian duct anomalies. AJR Am J Roentgenol 2012;198(2):302–310.
- Trolano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology 2004; 233(1):19–34.
- The American Fertility Society classifications of adnexal adhesions, distal tubal obstruction, tubal occlusion secondary to tubal ligation, tubal pregnancies, Müllerian anomalies and intrauterine adhesions. Fertil Steril 1988; 49:944–955.
- Olpin JD, Heilbrun M. Imaging of müllerian duct anomalies. Clin Obstet Gynecol 2009;52(1):40–56.
- Li S, Qayyum A, Coakley FV, Hricak H. Association of renal agenesis and mullerian duct anomalies. J Comput Assist Tomogr 2000;24(6):829–834
- Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update 2011;17(6):761–771.
- Hall-Craggs MA, Williams CE, Pattison SH, et al. Mayer-Rokitansky-Kuster-Hauser syndrome: diagnosis with MR imaging. Radiology 2013;269(3).
- Giusti S, Fruzzetti E, Perini D, Fruzzetti F, Giusti P, Bartolozzi C, et al. Diagnosis of a variant of Mayer-Rokitansky-Kuster-Hauser syndrome: useful MRI findings. Abdom Imaging. 2011;36:753–55.
- Fedele L, Bianchi S, Marchini M, Mezzopane R, DiNola G, Tozzi L. Residual uterine septum of less than 1 cm after hysteroscopic metroplasty does not impair reproductive outcome. Hum Reprod 1996; 11:727–729.