Adnexal Lesions: O-RADS MRI
Authors: Krista Suarez-Weiss, MD, Kristine Burk, MD, Atul Shinagare, MD
Date: February 23, 2021
| Peritoneal nodularity or irregular thickening | ORADS 5 | ||||||
| NO peritoneal nodularity or irregular thickening | Follicle or corpus luteum or hemorrhagic cyst <3cm in premenopausal women | ORADS 1 | |||||
| NOT follicle or corpus luteum or hemorrhagic cyst <3cm in premenopausal women | Lipid content | NO large volume enhancing solid tissue | ORADS 2 | ||||
| Large volume enhancing solid tissue | ORADS 4 | ||||||
| NO lipid content | NO enhancing solid tissue | Unilocular cyst | NO wall enhancement | ORADS 2 | |||
| Wall enhancement | Simple or endometriotic fluid | ORADS 2 | |||||
| Proteinaceous, hemorrhagic, or mucinous fluid | ORADS 3 | ||||||
| Multilocular cyst | ORADS 3 | ||||||
| Enhancing solid tissue (papillary projection, mural nodule, irregular septation/wall, larger solid portions) | Homogeneously T2 and DWI dark | ORADS 2 | |||||
| NOT T2/DWI dark | DCE: Low Risk TIC | ORADS 3 | |||||
| DCE: Intermediate Risk TIC Non-DCE: Hypo/isoenhancing to myometrium at 30-40s |
ORADS 4 | ||||||
| DCE: High Risk TIC Non-DCE: Hyperenhancing to myometrium at 30-40s |
ORADS 5 | ||||||
Quick Links:
- Risk Stratification System hyperlink: https://www.acr.org/-/media/ACR/Files/RADS/O-RADS/O-RADS-MR-Risk-Stratification-System-Table-September-2020.pdf
- Lexicon hyperlink: https://www.acr.org/-/media/ACR/Files/RADS/O-RADS/O-RADS-MR-Lexicon-Terms-Table-November-2020.pdf
- MR O-RADS Calculator hyperlink: http://oradsmricalc.com/
1. Major Categories
| Category | Term | Definition | Example |
|
1a. Physiological observations |
Follicle | Simple cyst ≤ 3 cm in pre-menopausal women. A follicle is hyperintense on T2WI, hypointense on T1WI, and does not enhance. | 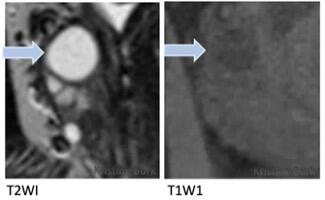 |
| Corpus luteum (CL) | Cyst ≤ 3 cm with an enhancing crenulated wall on subtracted post-contrast T1WI, +/- blood flow or hemorrhagic contents. | 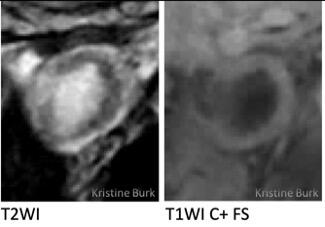 |
|
| 1b. Lesions (not physiologic) |
Unilocular Cyst | Single locule, without or without solid tissue. | 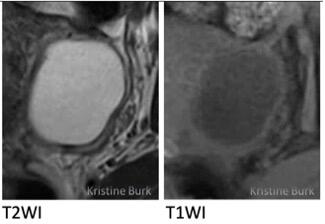 |
| Multilocular Cyst | More than one locule, with or without solid tissue. |  |
|
| Solid tissue | Conforms to one of the following morphologies and enhances: papillary formations, mural nodules, irregular cyst wall/septations, and solid portion. | See below | |
| Other solid components, not considered solid tissue | Smooth wall/septation, clot/debris/fat | See below |
2. Size
| Category | Term | Definition |
| Maximum diameter | Largest diameter of the lesion and/or solid component in any imaging plane. |
3. Shape or Contour of Solid Lesion or Solid Tissue
| Category | Term | Definition | Example |
| 3a. | Smooth | Regular or even margin of a solid lesion or solid tissue | 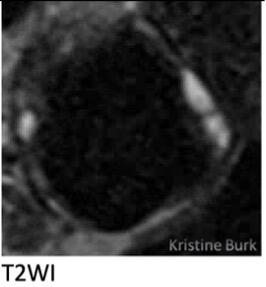 |
| 3b. | Irregular | Uneven margin of a solid lesion or solid tissue |  |
4. Signal Intensity
| Category | Term | Definition |
| 4a. | Homogenous | |
| Heterogeneous | ||
| 4b. | T2 Hypointense | Signal intensity ≤ iliopsoas muscle |
| T2 Intermediate | Signal intensity between that of iliopsoas muscle and CSF | |
| T2 Hyperintense | Signal intensity ≥ CSF | |
| 4c. | T1 Hypointense | Signal intensity that of simple fluid |
| T1 Intermediate | Signal intensity ≥ iliopsoas muscle but < fat | |
| T1 Hyperintense | Signal intensity ≥ fat | |
| 4d. | DWI High B-value Low signal | Adnexal lesion with signal similar to urine or cerebral spinal fluid |
| DWI High B-value High signal | Adnexal lesion with signal clearly higher than urine or CSF |
5. Lesion Components
| Category | Term | Definition | Example |
| 5a. Cystic fluid descriptors | Simple fluid | Fluid content that follows CSF or urine on all sequences: hyperintense on T2WI and hypointense on T1W1 | 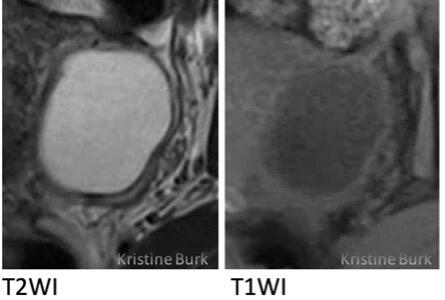 |
| Hemorrhagic fluid | Content can be variable depending on age |  |
|
| Fluid-fluid level | Appearance when the non-dependent fluid component has a different signal intensity from the dependent fluid component with horizontal delineation (blue arrow) | ||
| Endometriotic fluid | Content is hypointense on T2WI and hyperintense on T1WI | ||
| Shading | Cyst fluid that is hypointense on T2WI; the extent of hypointense T2 signal intensity may be homogenous, variable within the cyst or graduated and dependent | 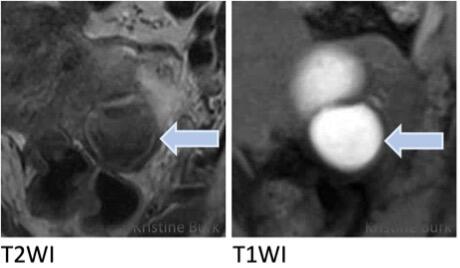 |
|
| Proteinaceous fluid | Content is variable on T2WI and variably hypointense on T1WI | 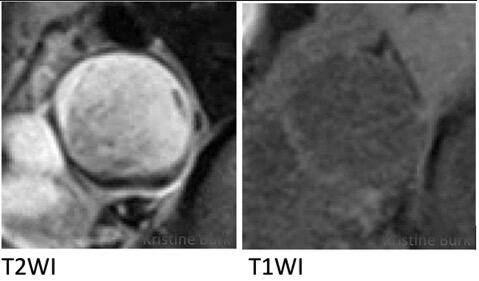 |
|
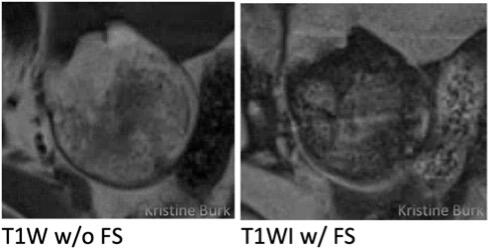
| Fat or lipid containing fluid | Hyperintense on T2WI and hyperintense on T1WI, and loses signal on fat saturated images | 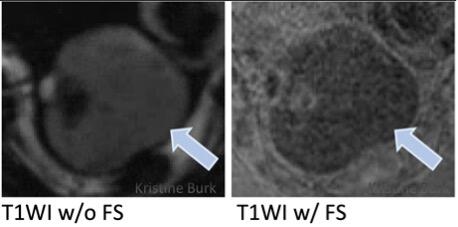 |
|
| 5b. Solid tissue descriptors (solid tissue enhances and conforms to one of the listed morphologies) |
Papillary projection | Enhancing solid component arising from the inner/outer wall or septation of an adnexal lesion, with a branching architecture | 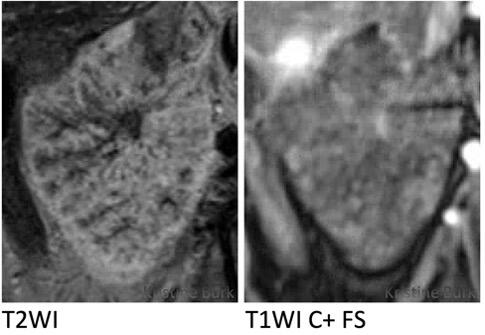 |
| Mural nodule | Enhancing solid component, measuring ≥ 3 mm, arising from the wall or septation of an adnexal lesion, with nodular appearance | 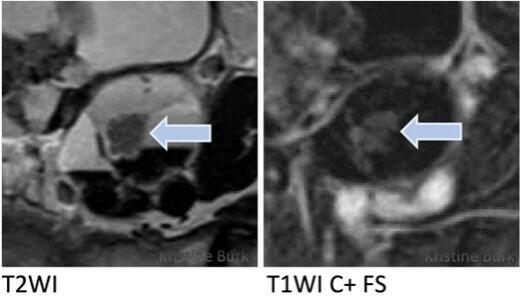 |
|
| Irregular septation | Enhancing linear strand that runs from one internal surface of the cyst to the contralateral side demonstrating an uneven margin (blue arrow) | 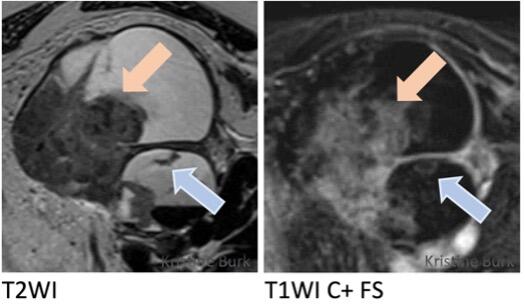 |
|
|
Larger solid portion |
Enhancing component of an adnexal lesion that does not fit into the categories of papillary projection, mural nodule, or irregular septation/wall (orange arrow) | ||
| Irregular wall | Enhancing cyst wall demonstrating an uneven margin | 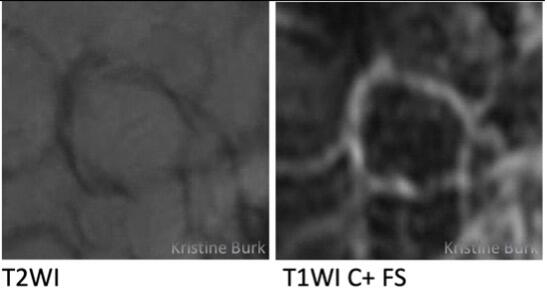 |
|
| Other solid components, not considered solid tissue | Smooth septations/wall | Even contour or margin with no irregularities, mural nodules or papillary projections | 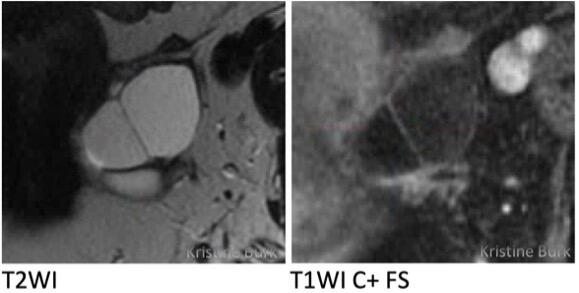 |
| Blood, clot, non-enhancing debris and fibrin strands | Solid-appearing material within a cyst that does not enhance | 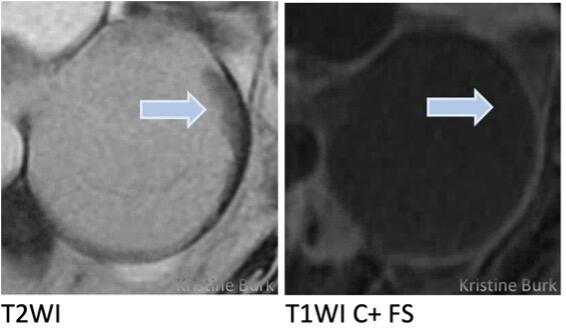 |
|
| Fat | Lipid-containing material that does not enhance |
|
|
| Hair, calcification, and a Rokitansky nodule | Other components of a dermoid not considered solid tissue |
6. Enhancement: T1W1 post-contrast
| 6a. Dynamic contrast enhancement with time intensity curves | Low risk curve | Solid tissue shows minimal and gradual increase in enhancement over time with no well-defined shoulder and no plateau |  |
| Intermediate risk curve | Enhancement of the solid tissue within the adnexal lesion with an initial slope less than the myometrium, moderate increase in signal intensity with a plateau | ||
| High risk curve | Enhancement of the solid tissue within the adnexal lesion with an initial slope greater than the myometrium, marked increase in signal intensity with a plateau | ||
| 6b. Non-dynamic contrast enhancement at 30-40 seconds post-injection | Less than or equal to the myometrium | Enhancement of the solid tissue within the adnexal lesion (blue arrow) is hypoenhancing to the outer myometrium (orange arrow) at 30-40 seconds post-contrast injection |  |
| Greater than myometrium | Enhancement of the solid tissue within the adnexal lesion (blue arrow) is equal to or greater than the outer myometrium (orange arrow) at 30-40 seconds post-contrast injection | 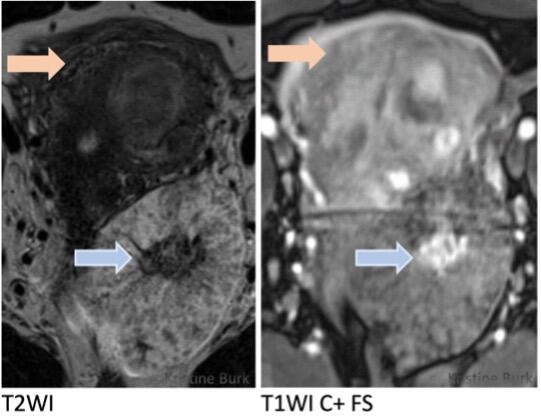 |
7. General and Extra-Ovarian Findings
| 7a. Peritoneal fluid | Physiologic | Small amount of fluid inside the pouch of Douglas or cul-de-sac or between the uterus and bladder | |
| Ascites | Fluid outside the pouch of Douglas or cul-de-sac or fluid extending beyond the space between the uterus and bladder | ||
| 7b. Fallopian tube descriptors | Tubular | Substantially longer in one dimension than in the two perpendicular dimensions | 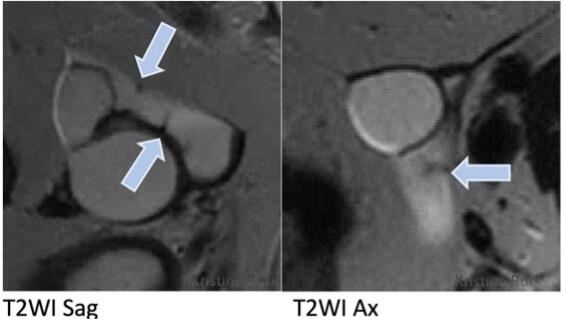 |
| Endosalpingeal folds | Incomplete septations or short round projections, orthogonal to the length of the tube | ||
| 7c. | Peritoneal inclusion cyst | Cyst following contour of adjacent pelvic organs; or normal ovary at the edge of/or surrounded by a cystic mass |  |
| 7d. Ovarian torsion | Twisted pedicle | Swirling appearance of the broad ligament or ovarian pedicle | 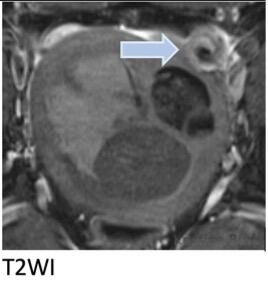 |
| Massive ovarian edema | Enlarged ovary with edematous central stroma |  |
|
| Ovarian infarction | Lack of enhancement of the ovary on T1WI post-contrast (blue arrow; orange arrow shows normal left ovary for reference) |  |
|
| 7e. Peritoneal thickening, nodules | Thickening, smooth | Uniform thickening, without focal nodularity | |
| Thickening, irregularity | Nonuniform thickening or focal areas of nodularity |
- O-RADS MRI 0: An incomplete evaluation
- O-RADS MRI 1: Normal Ovaries
- No ovarian lesion
- Ovarian follicle, defined as a simple cyst ≤ 3 cm in a premenopausal* woman
- Hemorrhagic cyst ≤ 3 cm in a premenopausal woman
- Corpus luteum +/- hemorrhage ≤ 3 cm in a premenopausal woman
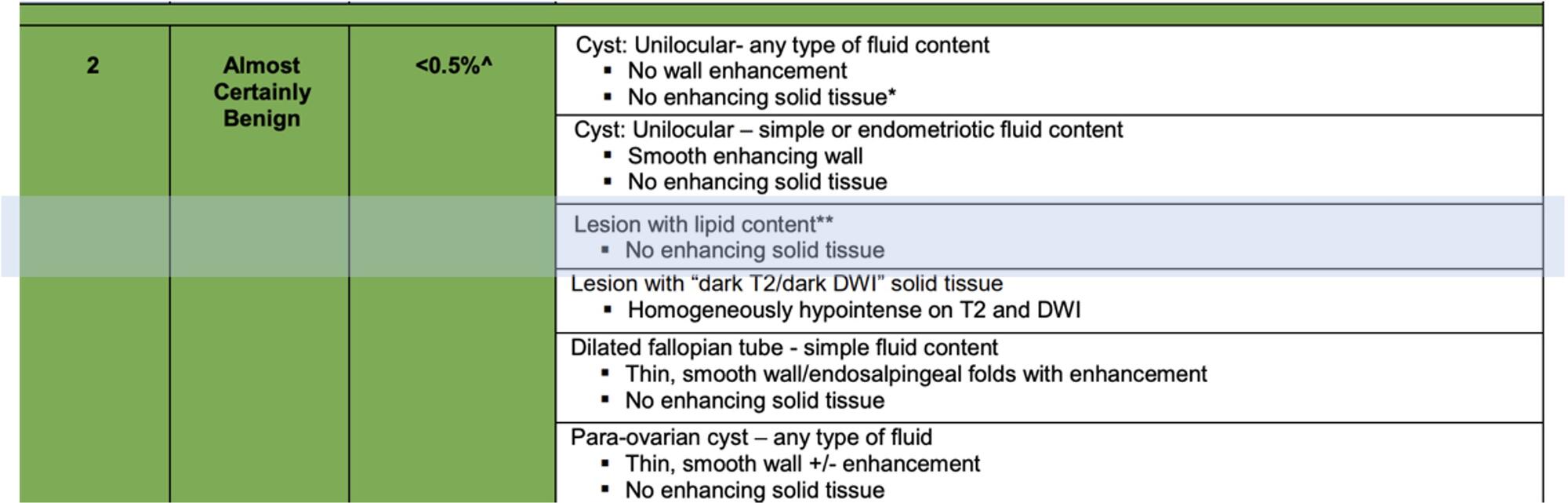
- O-RADS MRI 2: Almost certainly benign (<0.5% risk of malignancy)
- Unilocular cyst with no enhancing solid tissue**
- If no wall enhancement, may have any type of fluid content
- If smooth wall enhancement, may have simple or endometriotic fluid content
- Lesion with lipid content and:
- No enhancing solid tissue
- Only minimal enhancement of the Rokitansky nodule
- Lesion with homogenously hypointense solid tissue on T2WI and DWI
- Dilated fallopian tube with simple fluid content (hydrosalpinx) but no enhancing solid tissue. May have a thin, smooth wall/endosalpingeal folds with enhancement.
- Para-ovarian cyst with no enhancing solid tissue. May have any type of fluid content, and may have a thin, smooth wall +/- enhancement.
- Unilocular cyst with no enhancing solid tissue**
- O-RADS MRI 3: Low risk of malignancy (~ 5%)
- Unilocular cyst with no enhancing solid tissue, smooth wall enhancement, and proteinaceous, hemorrhagic, or mucinous fluid content
- Multilocular cyst with no enhancing solid tissue or lipid content. May have any type of fluid content, and may have smooth septae and wall with enhancement
- Lesion with solid tissue (excluding T2 and DWI dark) with low-risk time intensity curve on DCE MRI***
- Dilated fallopian tube with no enhancing soft tissue nodule and:
- Non-simple fluid and thin walls/folds
- Simple fluid with thick, smooth walls/folds
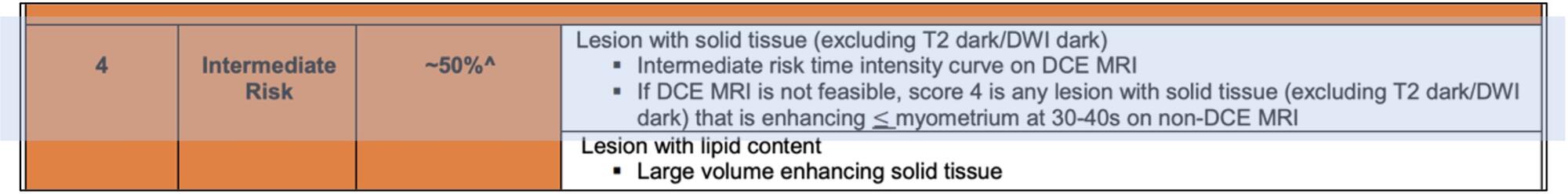
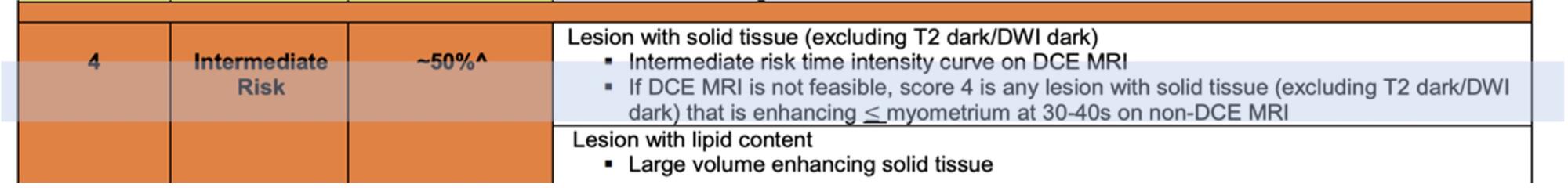
- O-RADS MRI 4: Intermediate risk of malignancy (~ 50%)
- Lesion with solid enhancing tissue (excluding T2 and DWI dark) with:
- Intermediate-risk time intensity curve on DCE MRI****
- If DCE MRI is not feasible, any lesion with enhancement ≤ myometrium at 30-40s on non-DCE MRI
- Lesion with lipid content and large volume enhancing solid tissue
- Lesion with solid enhancing tissue (excluding T2 and DWI dark) with:
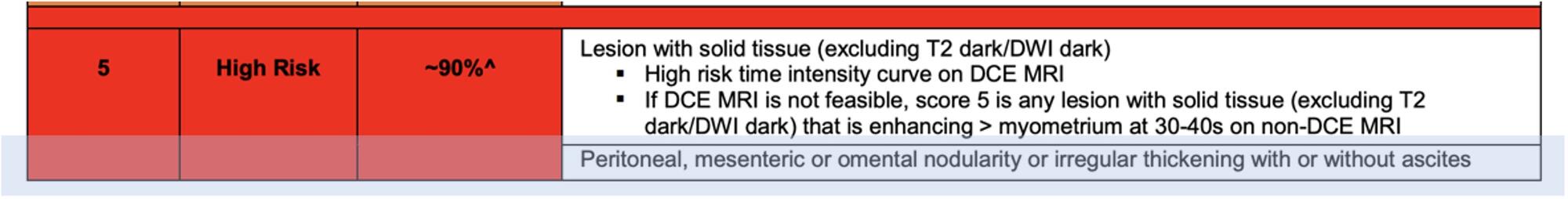
- O-RADS MRI 5: High risk of malignancy (~ 90%)
- Lesion with solid tissue (excluding T2 and DWI dark with:
- High-risk time intensity curve on DCE MRI*****
- If DCE MRi is not feasible, any lesion with enhancement > myometrium at 30-40s on non-DCE MRI
- Peritoneal, mesenteric, or omental nodularity or irregular thickening with or without ascites
- Lesion with solid tissue (excluding T2 and DWI dark with:
*Women are categorized as pre- or postmenopausal, with postmenopausal defined as ≥ 1 year of amenorrhea
**Solid tissue is defined as a lesion component that enhances and has one of the following morphologies: papillary projection, mural nodule, irregular septation/wall, or other larger solid portions that do not conform to the aforementioned morphologies.
***Low-risk curve = minimal and gradual increase in signal over time with no well-defined shoulder and no plateau
****Intermediate-risk curve = initial slope less than myometrium, moderate increase in signal intensity with a plateau
*****High-risk curve = initial slope greater than myometrium, marked increase in signal intensity with a plateau
When lesions can be confidently diagnosed by MRI features, the final radiological diagnosis can be reported without an O-RADS risk stratification score assigned.
An online O-RADS MRI calculator tool2 to aid in lesion characterization and O-RADS MRI assignment can be found at http://www.oradsmricalc.com.
Adnexal Findings:
For each adnexal lesion, describe:
- Size: Maximum diameter in any plane
- Morphology:
- Unilocular cyst without solid component
- Multilocular cyst without solid component
- Cystic with solid component
- Solid
- Cystic component (if applicable):
- Fluid descriptors: simple; non-simple fluid (hemorrhagic, endometriotic, proteinaceous, fat or lipid-containing).
- Signal descriptors: homogeneous; heterogeneous
- If present, describe fluid-fluid level/shading and smooth wall or septal enhancement.
- Solid tissue (if applicable):
- Solid tissue descriptors: irregular septation or wall; papillary projection; mural nodule; large solid tissue
- Signal descriptors: T2 intensity; high b value DWI signal; enhancement less than/equal to OR greater than outer myometrium at 30-40 seconds post-contrast injection
- Other solid component (if applicable):
- Smooth wall/septation, clot/debris, fat, hair, calcification, Rokitansky nodule
- Lipid component: Describe if present
Extra-adnexal Findings:
If present, include: ascites; peritoneal or omental stranding, thickening or nodularity.
Impression:
Lesion 1: ____. (O-RADS MRI __).
Lesion 2: ____. (O-RADS MRI __).
O-RADS MRI (Ovarian Imaging Reporting and Data System) assessment utilizes a 5-point scale to indicate the likelihood of malignancy based on a combination of multi-parametric MRI findings.
O-RADS MRI 0: Incomplete evaluation.
O-RADS MRI 1: Normal ovaries.
O-RADS MRI 2: Almost certainly benign (<0.5% PPV for malignancy).
O-RADS MRI 3: Low risk (~5% PPV for malignancy).
O-RADS MRI 4: Intermediate risk (~50% PPV for malignancy).
O-RADS MRI 5: High risk (~90% PPV for malignancy).
PPV = positive predictive value
Reference: Thomassin-Naggara I, Poncelet E, Jalaguier-Coudray A, et la. Ovarian-adnexal reporting data system magnetic resonance imaging (O-RADS MRI) score for risk stratification of sonographically indeterminate adnexal masses. JAMA Netw Open. 2020;3(1):e1919896.
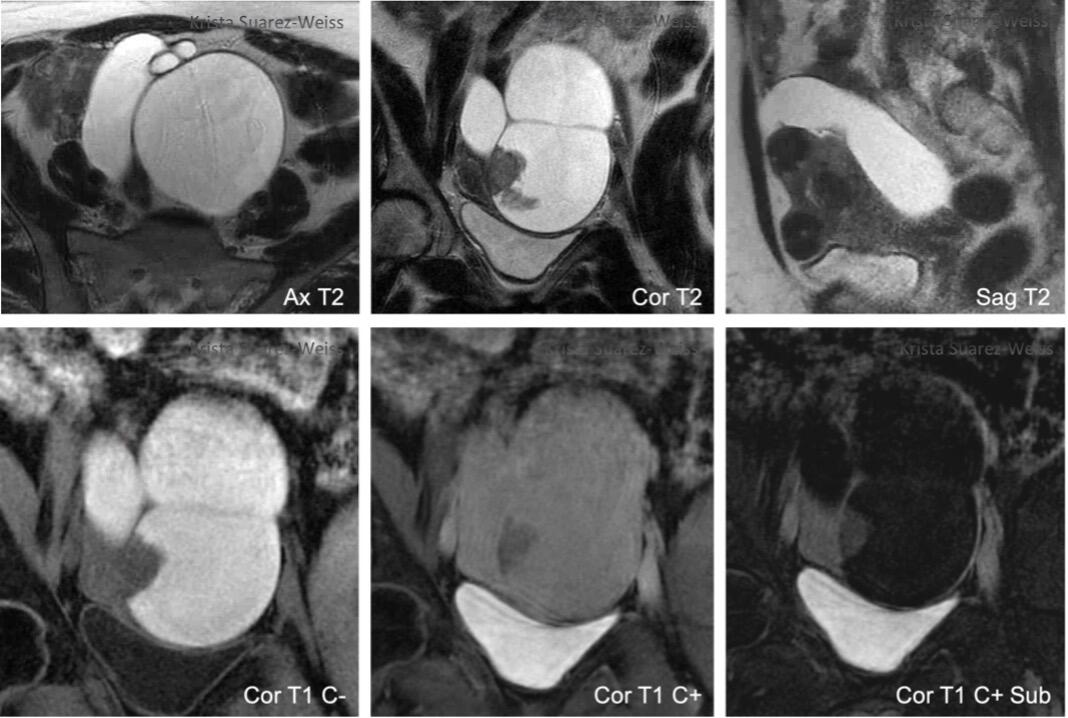
Case 1
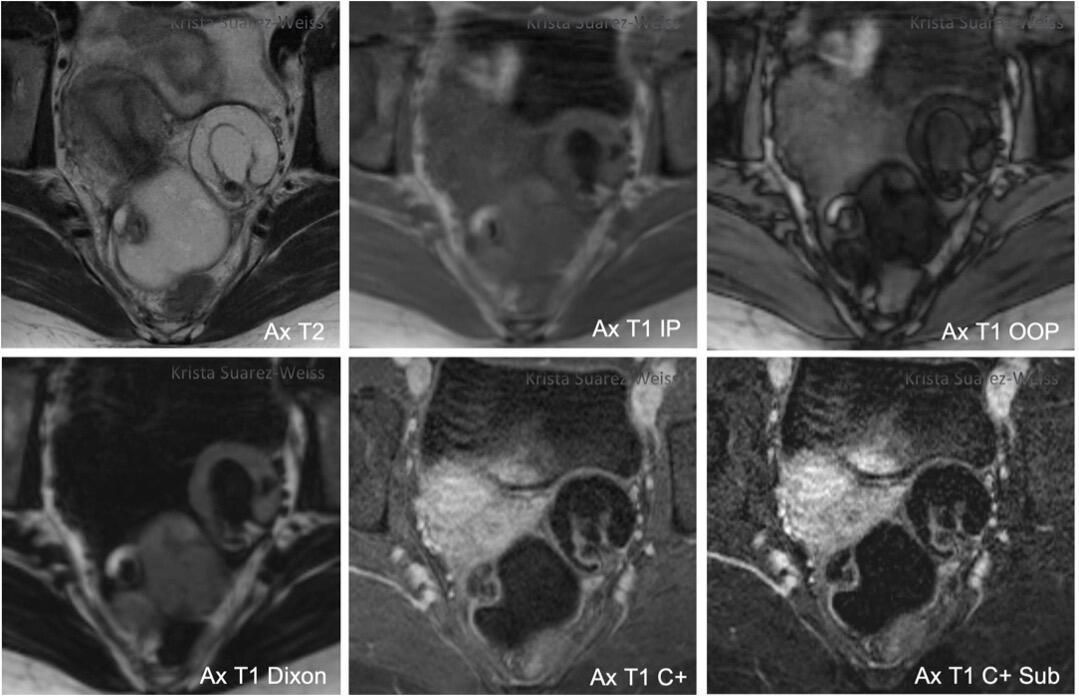
Lexicon Terms: Cystic lesion; non-simple fluid – fat or lipid-containing fluid; without solid tissue
Report Impression: Bilateral cystic lesions with lipid content without enhancing solid tissue, compatible with O-RADS MRI score 2 (almost certainly benign).
Pathology: Bilateral dermoid cysts.
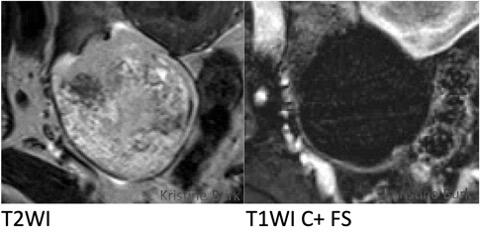
Case 2
Lexicon Terms: Cystic lesion; non-simple fluid – hemorrhagic fluid; solid tissue – mural nodule; tubular
Report Impression: Cystic adnexal lesion with solid tissue that enhances less than the outer myometrium, compatible with O-RADS MRI score 4 (intermediate risk).
Pathology: Serous adenocarcinoma likely arising from the fallopian tube.
 Case 3
Case 3

Lexicon Terms: Cystic lesion; simple fluid; solid tissue – mural nodule
Report Impression: Cystic adnexal lesion with enhancing solid tissue (mural nodule). Given enhancement less than the uterine myometrium, the lesion is classified as O-RADS MRI 4.
Pathology: Borderline serous cystadenoma.
Case 4
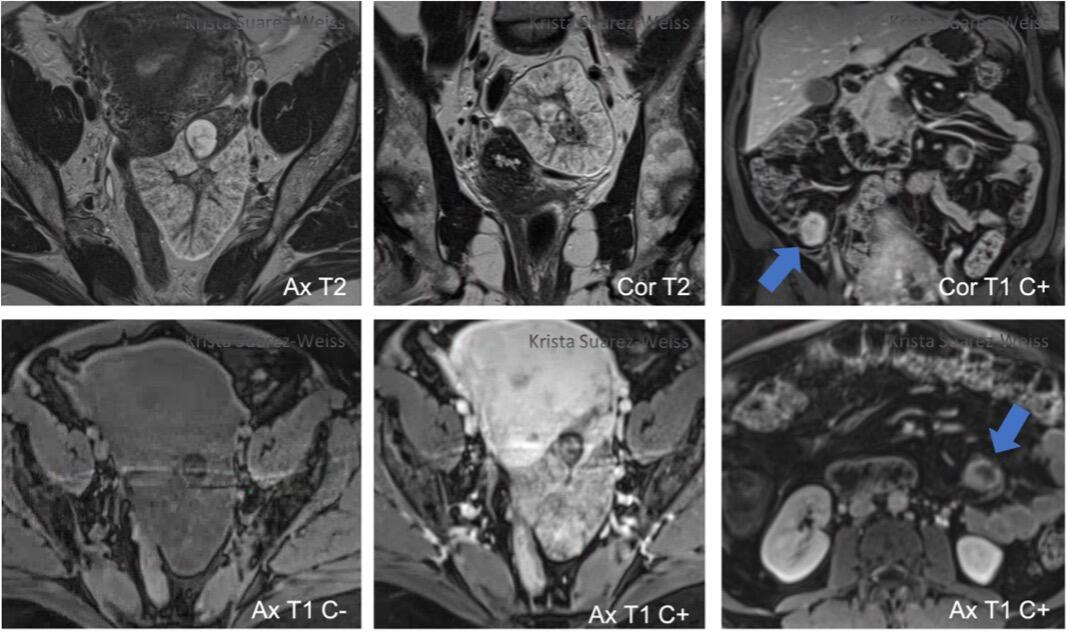
Lexicon Terms: Solid lesion; smooth shape/contour; heterogeneous; T2 hyperintense; T1 hypointense; peritoneal nodules
Report Impression: Adnexal lesion with solid tissue and peritoneal nodularity, compatible with O-RADS MRI score 5 (high risk).
Pathology: Borderline serous cystadenoma.
- Thomassin-Naggara I, Poncelet E, Jalaguier-Coudray A, et la. Ovarian-adnexal reporting data system magnetic resonance imaging (O-RADS MRI) score for risk stratification of sonographically indeterminate adnexal masses. JAMA Netw Open. 2020;3(1):e1919896.
- O-RADS MRI Lexicon Categories, Terms and Definitions. Release date: November 2002. https://www.acr.org/-/media/ACR/Files/RADS/O-RADS/O-RADS-MR-Lexicon-Terms-Table-November-2020.pdf
- O-RADS MRI Stratification System Table. Release date: September 2020. https://www.acr.org/-/media/ACR/Files/RADS/O-RADS/O-RADS-MR-Risk-Stratification-System-Table-September-2020.pdf