Superficial Endometriosis Implants (SIE)
|
Superficial Endometriosis Implants: |
Deep Infiltrating Endometriosis (DIE)
|
|||||
|
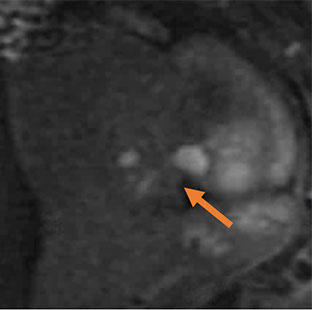
(1) Active glandular morphology
|
|
||||
|
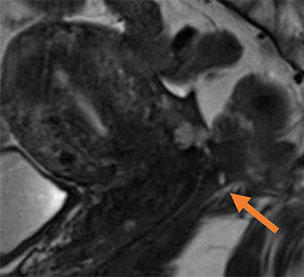
(2) Chronic stromal fibrotic morphology
|
Chronic Stromal Fibrotic Deep Infiltrating Endometriosis: |
||||
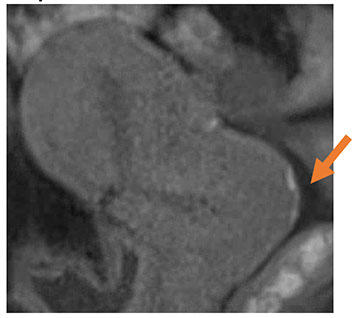
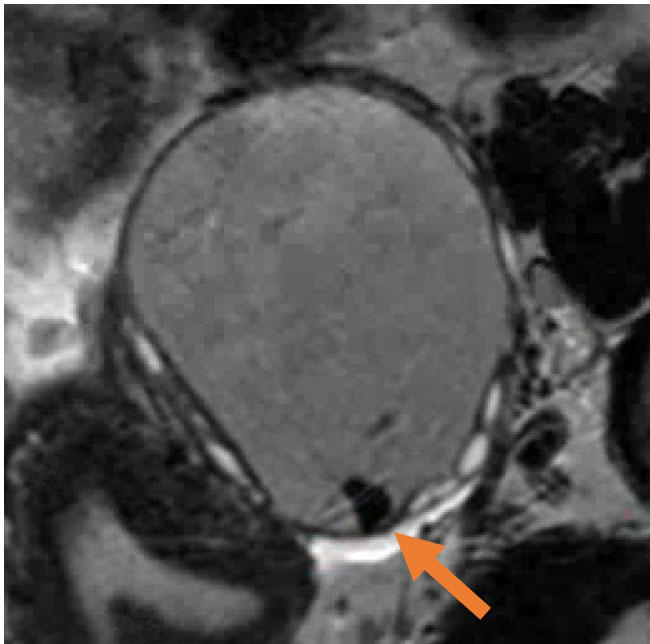
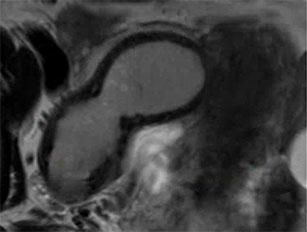
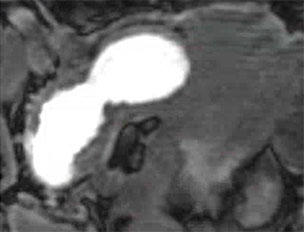
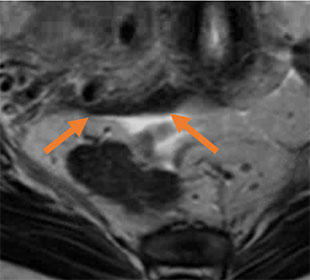
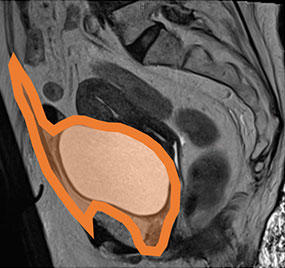
Endometriomas
|
|||||||||
|
|
||||||||
Anterior Compartment Contents
|
 |
Middle Compartment Contents
|
 |
Posterior Compartment Contents
|
 |
Anterior Compartment
|
Bladder
|
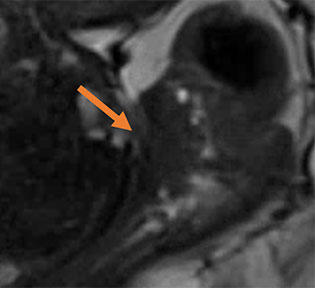
Active Glandular DIE of the Bladder:
|
||||||||
|
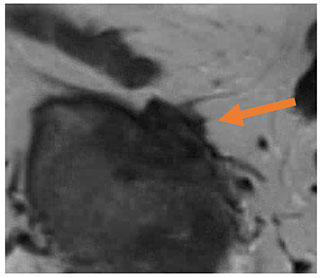
Ureters
|
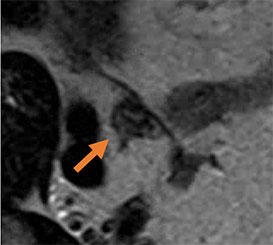
Intrinsic Chronic Stromal Fibrotic DIE of the Ureter with Mild Hydroureteronephrosis:
|
||||||||
|
Vesicouterine Space
|
Chronic Stromal Fibrotic DIE with Obliteration of the Vesicouterine Space:
|
Middle Compartment
|
Vagina
|
Active Glandular DIE of the Posterior Vaginal Forinx:
|
||||
|
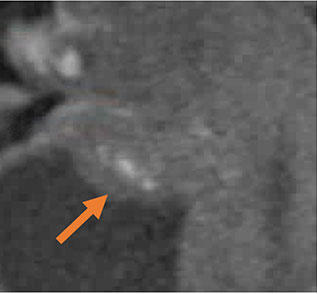
Fallopian Tubes
|
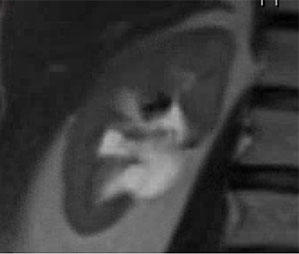
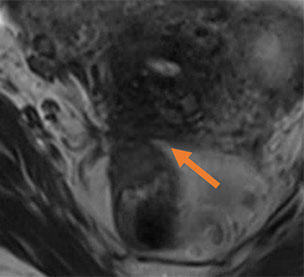
Hematosalpinx:
|
||||
|
Uterus
|
Mixed Active Glandular and Chronic Stromal Fibrotic DIE of the Torus Uterinus:
|
Posterior Compartment
|
Rectouterine/Cervical Space
|
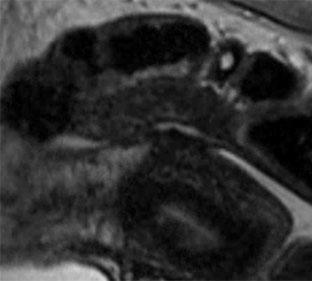
Chronic Stromal Fibrotic DIE of the Rectocervical Space:
|
||||||||||
|
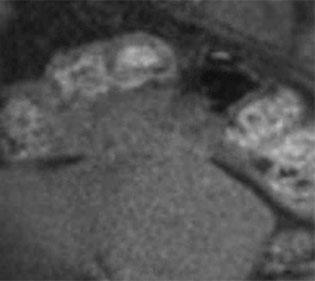
Uterosacral Ligaments
|
|
||||||||||
|
Rectosigmoid Colon
|
Chronic Stromal Fibrotic DIE of the Rectum
|
Key sequences:
- To evaluate for SEI = T1 weighted fat-saturated axial and sagittal
- To evaluate for DIE = T2 weighted non-fat-saturated axial, sagittal, and coronal
- To evaluate for endometriomas = Both listed above
- To evaluate for malignancy or infection: DWI/ADC and contrast enhanced T1 weighted images
Additional considerations:
- Use of an anti-peristaltic agent is highly recommended to minimize bowel motion artifact
- 0.5-1 mg glucagon, either IM or injected IV over 1 minute
- Hyoscyamine sulfate SL can be used in patients with a glucagon contraindication
- Vaginal distention with 60 cc of ultrasound gel is conditionally recommended
- typically injected by the patient
- Rectal distension 60-180 cc of ultrasound gel is conditionally recommended
- typically injected by a physician or other trained medical personnel
- Moderate bladder distension is conditionally recommended
Describe the following:
- Uterus:
- Version and flexion (always)
- Adenomyosis or adenomyoma (if present)
- Adnexa:
- Location in the pelvis (always)
- Are the ovaries tethered or displaced?
- Endometrioma (if present)
- Hydrosalpinx or hematosalpinx (if present)
- Location in the pelvis (always)
- Superficial endometriosis implants (if present)
- Compartment and location
- Deep endometriosis implants (if present)
- Compartment and location
- Morphology (active glandular or chronic stromal fibrotic)
- Size of implant
- Space obliteration/tethering of adjacent organs (if present)
- Organ invasion (if present, with individual organ considerations as detailed above)
- Superficial endometriosis implant – endometriosis implant with < 5 mm of peritoneal invasion
- Deep infiltrating endometriosis – endometriosis implant with > 5 mm of peritoneal invasion
- Active glandular DIE – morphology of deep infiltrating endometriosis in which hemorrhagic glandular and cystic tissue predominates
- Chronic stromal fibrotic DIE – morphology of deep infiltrating endometriosis in which fibrosis and smooth muscle hypertrophy predominates
- Tethering/obliteration – fibrotic scarring across a peritoneal or retroperitoneal space, bringing adjacent organs into fixed contact with one anothe
- Endometrioma – thick walled ovarian or paraovarian cyst containing blood of varying age
- Extrinsic ureteral involvement – DIE that abuts the ureter causing tethering and a resultant angulated course, but no invasion
- Intrinsic ureteral involvement – DIE that invades the wall of the ureter resulting in luminal narrowing and obstruction/hydroureteronephrosis
- Uterine version – angle of the uterus relative to the angle of the vagina: anteversion or retroversion
- Uterine flexion – angle of the uterine body relative to the angle of the cervix: anteflexed or retroflexed
- Torus uterinus – junction of the uterine corpus and the cervix along the posterior serosa/origin of the uterosacral ligaments
- Vaginal Fornix – most superior reflection of the vaginal wall/recess of the vaginal lumen, formed by the protrusion of the cervix into the vaginal vault
- Hematosalpinx – a Fallopian tube filled with hemorrhagic products, implies the presence of endometriosis implants within the tube, tough these are not always seen
The Signs:
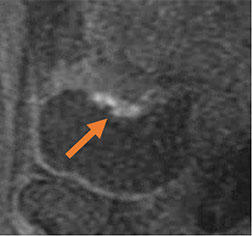
- T2 Shading – decreased signal seen within an endometrioma on T2 weighted images, may or may not have a layered appearance
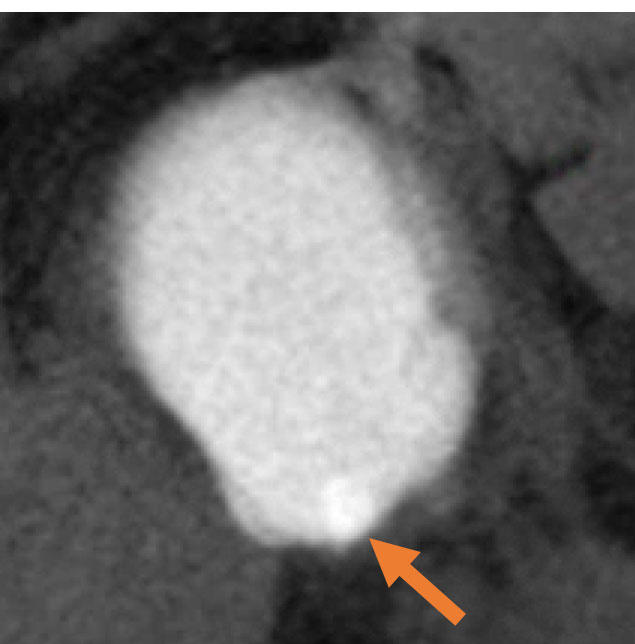
- T2 dark spot sign – T2 dark/T1 bright nodule of inspissated blood products that may be found at the edge of an endometrioma
- Kissing ovaries – medialization and tethering of the ovaries together, usually in the rectouterine space though can also occur in the vesicouterine space, implies paraovarian chronic stromal fibrotic DIE
- P Jha, M Sakala, LP Chamie, M Feldman et al., Endometriosis MRI lexicon: consensus statement from the Society of Abdominal Radiology endometriosis disease-focused panel. Abdominal Radiology (2019) 10.1007/s00261-019-02291-x.
- A Darvishzadeh, W McEachern, TK Lee, P Bhosale et al., Deep pelvic endometriosis: a radiologist’s guide to key imaging features with clinical and histopathologic review. Abdominal Radiology (2016) 41:2380-400.
- Kaniewska M, Goloft P, Heubner M et al., Suspensory ligaments of the female genital organs: MRI evaluation with intraoperative correlation. Radiographics (2018) 38:2195-2211).
- A Tong, WM VanBuren, L Chamie et al., Recommendations for MRI technique in the evaluation of pelvic endometriosis: consensus statement from the Society of Abdominal Radiology endometriosis disease-focused panel. Abdominal Radiology (2020) 45:1569-86.
- A Jaramillo-Cardoso, AS Shenoy-Bhangle, WM VanBuren et al., Imaging of gastrointestinal endometriosis: what the radiologist should know. Abdominal Radiology (2020) 45:1694-1710.
- A Agely, C Bolan, A Metcalfe et al., Genitourinary manifestations of endometriosis with emphasis on the urinary tract. Abdominal Radiology (2020) 45:1711-22.